Abstract
Introduction: Murine double minute 2 (MDM2) is the primary negative regulator of the tumor suppressor protein, p53. Navtemadlin (KRT-232), a potent, selective, orally available MDM2 inhibitor, is being evaluated in the phase 3 BOREAS trial of patients with relapsed/refractory myelofibrosis (MF; NCT03662126) and in phase 1b/2 trials in various tumor types. In preclinical studies, navtemadlin has overcome MDM2 dysregulation and has restored p53 activity to drive apoptosis in TP53WT malignancies. The primary determinant of tumor cell sensitivity to navtemadlin is TP53 mutation status. Because MDM2 is often overexpressed and p53 mutations are less common in treatment-naïve acute myeloid leukemia (AML) and MF, navtemadlin represents a rational therapeutic candidate for these malignancies (Prokocimer et al. Blood. 2017). The present study aims to elucidate the effects of navtemadlin on proteins downstream of p53 and synergy of navtemadlin with the FLT3 inhibitor gilteritinib in myeloid malignancies.
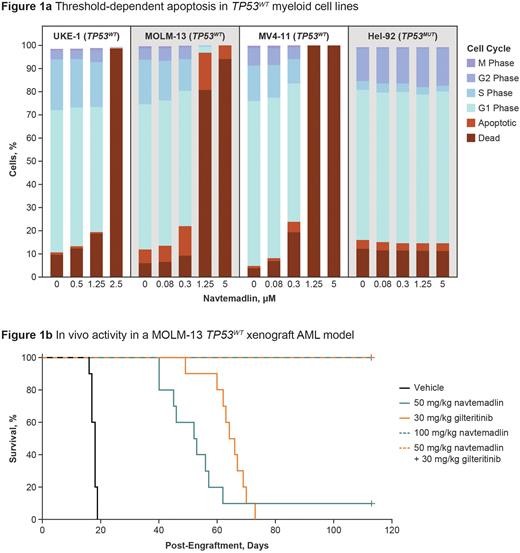
Methods: Cell viability was evaluated in three TP53WT myeloid cell lines, MOLM-13 (FLT3 AML), MV-4-11, and UKE-1, and one TP53MUT myeloid cell line, HEL-92, treated with 1-10 µM navtemadlin for 72 h. Growth inhibition was determined using the ATP-based Cell Titer Glo assay. The treatment effect on cell cycle progression, BCL-2 family proteins, and apoptosis was determined by flow cytometry. The effects of navtemadlin (0.5-1 µM) + gilteritinib (0.5-1 µM) were assessed in MOLM-13 and MV-4-11 (TP53WT and TP53MUT clones) and visualized using Combenefit. A MOLM-13 TP53WT mouse xenograft model was used to assess in vivo activity. Engrafted mice were randomly assigned to one of five treatment groups (n=10 each): vehicle control, 30 mg/kg gilteritinib, 50 mg/kg navtemadlin, 50 mg/kg navtemadlin + 30 mg/kg gilteritinib, or 100 mg/kg navtemadlin. Mice were treated orally once a day until the mice met early removal criteria or the study was terminated. Survival was measured by the percentage of mice in each group that remained alive at the end of the study.
Results: Navtemadlin exposure led to dose-dependent growth inhibition in the TP53WT myeloid cell lines MOLM13, MV-4-11, and UKE-1 with an EC90 of 2-6 µM. Conversely, no growth inhibition was observed in the TP53MUT myeloid cell line HEL-92, up to 10 µM of navtemadlin. Assessment of cell cycle progression following navtemadlin exposure showed the induction of threshold-dependent apoptosis in the TP53WT myeloid cell lines, but not in the TP53MUT myeloid cell line. The threshold at which a switch from p21-mediated cell-cycle arrest to p53-directed apoptosis occurs is illustrated in Figure 1a. Navtemadlin-induced apoptosis was indicated by a release of cytochrome c and increase in processed caspase-3. Clinically, a steady-state Cmax of 2-6 µM is achieved at therapeutically active and relevant doses of navtemadlin ≥180 mg given once a day on a 5-day or 7-day schedule in clinical trials, leading to maximum tumor cell death. To gain better insight into the contribution of BCL-2 family members alterations as an MOA for navtemadlin-induced apoptosis, expression levels of BCL-2 family members were evaluated in TP53WT myeloid cell lines. Navtemadlin increased levels of the effector pro-apoptotic proteins Bak, Bax, and Bim in leukemia cells. Synergy was observed in vitro for navtemadlin + gilteritinib in TP53WT, but not TP53MUT myeloid cell lines. Treatment with 100 mg/kg navtemadlin monotherapy and 50 mg/kg navtemadlin + gilteritinib combination led to prolonged survival in mice harboring MOLM-13 TP53WT xenografts, with all mice still alive at day 113 when the study was terminated (Figure 1b). In contrast, median survival times for the vehicle, 50 mg/kg navtemadlin monotherapy, and gilteritinib monotherapy groups were 18, 53, and 65 days, respectively.
Conclusion: Navtemadlin induces potent, threshold-dependent apoptosis in cell culture models of TP53WT myeloid malignancies at clinically relevant concentrations. Navtemadlin-induced p53 activity initiates apoptosis by activating the caspase cascade via cytochrome c release. Navtemadlin was shown to induce the expression of pro-apoptotic BCL-2 family proteins, key mediators in driving cell death. These pro-apoptotic effects translate to robust antitumor activity in xenograft models of TP53WT myeloid malignancies, with the navtemadlin + gilteritinib combination demonstrating synergy.
Disclosures
Clevenger:Kartos Therapeutics: Current Employment, Current holder of stock options in a privately-held company. Gulrajani:Kartos Therapeutics: Current Employment, Current holder of stock options in a privately-held company. Cheung:Kartos Therapeutics: Current Employment, Current holder of stock options in a privately-held company. Larkin:Gilead: Membership on an entity's Board of Directors or advisory committees. Covey:Kartos Therapeutics: Current Employment. Rothbaum:Quogue Capital: Current Employment; Iovance Biotherapeutics: Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees, Other: travel, accommodations, expenses; Acerta Pharma/Astra Zeneca: Current equity holder in publicly-traded company; Kartos Therapeutics: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees, Other: travel, accommodations, expenses, Patents & Royalties; Telios Pharma: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees, Other: travel, accommodations, expenses, Patents & Royalties; Quogue IP Holdings: Patents & Royalties. Byrd:Kura: Consultancy; Janssen: Consultancy; Vincerx: Consultancy, Current equity holder in private company, Current equity holder in publicly-traded company, Current holder of stock options in a privately-held company; Novartis: Consultancy; Syndax: Consultancy; Ohio State University: Patents & Royalties; Newave: Consultancy; AbbVie: Consultancy; AstraZeneca: Consultancy; Zencor: Research Funding; Pharmacyclics: Research Funding; Trillium: Consultancy.
OffLabel Disclosure:
Yes, navtemadlin (KRT-232) is an investigational small molecule inhibitor.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal